With Functioning Kidneys for All
The Atlantic , July 08, 2009
In February 2007, Garet Hil’s 10-year-old daughter came down with what looked like the flu: a persistent fever, vomiting, dizziness, fainting. On her third trip to the pediatrician, the doctor told the family to take her to the emergency room. There, a blood test delivered frightening news: her kidneys had shut down.
“They put us in an ambulance and rushed her to a nearby hospital that had a pediatric nephrology unit, which put her on dialysis immediately,” recalls Hil. “That saved her life.”
Unfortunately, dialysis also threatened to take over her life. As the long-term treatment for permanent kidney failure, dialysis is a good-news/ bad-news technology. It is life-preserving, but often debilitating and demoralizing—akin to saving polio patients with iron lungs, or treating cancer with never-ending chemotherapy. Dialysis patients are prone to anemia, bloating and weight gain, low blood pressure, and infection from their catheters. They gradually lose the ability to urinate and can drink very little (not very little alcohol—very little anything). Many children on dialysis suffer from stunted growth. Dialysis does not make patients well. It simply postpones their deaths.
“Yes, it keeps us alive, but this is not what living should be like,” wrote Bill “Epoman” Halcomb, the founder of the patient community at IHateDialysis.com. (Halcomb died in March 2007, after 13 years on dialysis. He was 34.) Dialysis patients typically spend three or four hours hooked up to a machine, three days a week, making work, school, or travel extremely difficult. “Tuesday, Thursday, and Saturdays I show up around 4:15 in the morning, and I’m on the machine by about 4:30 or so. It’s about 8:00 or 8:15 when I’m out of there,” Henry David, a 60-year-old Los Angeles business owner, explained to me in February. Why start well before dawn? “It’s my choice, because I want to have something of a life.”
The Hils wanted more than “something of a life” for their little girl, who turned out to have a rare genetic disorder called familial juvenile nephronophthisis, which causes the kidneys to develop incapacitating cysts. It has no cure, but one treatment can solve the problem for years, even decades: a kidney transplant.
Unlike dialysis patients, transplant recipients can live normal lives, with few restrictions besides the need for immunosuppressant drugs. Since getting a transplant in late May, David says, “I can eat anything I want to eat. I’ll be able to travel. I don’t need a nap every day. There’s no comparison.” Despite the high price of drugs, transplants overall cost less money—a lot less money—than long-term dialysis.
You might think that such a superior treatment would be standard. But kidneys are hard to come by. In the United States, more than 80,000 people are on the official waiting list, all hoping that someone will die in just the right circumstances and bequeath them the “gift of life.” Last year, only 16,517 got transplants: 10,550 with the cadaver organs allocated through the list, and 5,967 from living donors. More than 4,000 on the list, or about 11 a day, died. And the list gets longer every year.
For those who survive long enough to get transplants, the wait routinely lasts years. The odds are particularly bad in large cities. Take the nation’s largest transplant center, the University of California, San Francisco. In 2008, its surgeons did an impressive 347 kidney transplants, including 231 with organs from deceased donors. But 5,271 people are on UCSF’s waiting list—meaning that, relying entirely on deceased donors, they would expect to wait an average of almost 23 years. If, like Steve Jobs, who recently got a liver transplant in Memphis, you can travel great distances on short notice, you can register all over the country. But few kidney patients are that flexible. They wait, they get sicker, and, too often, they die.
With 300 million people in the United States, the numbers shouldn’t be so daunting. Eighty thousand people wouldn’t even fill the Rose Bowl. Surely we could find enough kidney donors to end the list. But solving that problem demands creativity, daring, and, above all, a sense of urgency—a radical break with the fatalism fostered by dialysis culture. Kidney patients ought to command the kind of outrage that demanded a cure for AIDS. The list doesn’t have to exist. It is a result not of medical necessity or economic constraints but of public ignorance, conscious policy, and complacent institutions. Too many people are suffering unnecessarily.
To end the list, we first have to give up the idea that “organ donor” means someone dead. Deceased donors are, of course, essential for hearts. But not for kidneys. And not enough people die in exactly the right way to meet the need for kidneys. The best estimate is that there are between 10,500 and 13,800 brain-dead potential organ donors each year. More than half already become donors, and not all their kidneys can be used. If every single person who died the right way became an organ donor, an optimistic estimate would be that 7,000 more kidneys a year would be available for transplant. Since the list is now increasing by 6,000 a year, that would be enough to end it—in 80 years.
And even those numbers understate the problem. Though the list is inflated with “inactive” patients who aren’t healthy enough for transplants at the moment but don’t want to lose their place in line, it does not include a host of others who would be good transplant candidates right away—nearly another 80,000, estimates a study published last year in the American Journal of Transplantation. “The potential need for kidneys is a lot greater than the waiting list itself,” says Arthur Matas, the director of the renal-transplant service at the University of Minnesota Medical School and a past president of the American Society of Transplant Surgeons.
Eighty years or 160 or merely 40. Whichever you pick, the number of deceased donors will never be enough. Any sense of urgency inevitably leads to the same conclusion: we need a lot more living donors.
Volunteering one of his kidneys was the obvious choice for Garet Hil, who wasn’t about to wait years as his little girl grew ever sicker. Like most people, he knew almost nothing about kidney disease or kidney transplants before his daughter got sick. “If you’d asked me how many kidneys I had, I wouldn’t have known I had two,” he says. A Wharton-educated management consultant and former CEO, he soon mastered the basics. Living with a single kidney is almost exactly like living with two; the remaining kidney expands to take up the slack. (When kidneys fail, they generally fail together; barring trauma or cancer, there’s not much advantage to a backup.) The main risk to the donor is the risk of any surgery. The kidney can now be removed laparoscopically, using tiny incisions and a fiber-optic camera to guide the surgeon, thus avoiding the huge abdominal slice and lengthy recovery time that used to be standard. Kidney donors don’t have to be close relatives of recipients, but they do need to have the right blood type. And kidneys from living donors tend to last many years longer than kidneys from deceased donors.
Since the current transplant system extols altruism, one way to end the list would be to find more altruists. With, say, 50,000 new living donors, deceased donation could easily pick up the slack. Again, the numbers aren’t that big. The Southern Baptist Convention includes 42,000 member churches; the United Methodist Church, whose Web site earlier this year featured the quote, “As United Methodists, we’re life savers,” counts more than 34,000 U.S. congregations. If each congregation produced just one new living donor, the waiting list would disappear. But kidney donation is a more visceral mission than mainstream religious groups want to contemplate. The only sect to adopt kidney donation as a formal cause is a tiny Australia-based group called Jesus Christians; instead of lauding them, critics point to their donations as evidence that they’re a cult.
Nor has the cause attracted much secular attention. Kidney disease is a low-profile, unglamorous problem, a disease that disproportionately strikes minorities and the poor. Its celebrity spokesman is blue-collar comedian George Lopez, who received a kidney from his wife. “It’s not AIDS, it’s not cancer,” says Jack Daly, who worked on kidney-related legislation when he was counsel for the Senate Judiciary Committee. “Kidney donation is not a very sexy issue.” Even uncontroversial bills sit around for years without action. “Seemingly, a member of Congress has to die to get an organ-donation-related bill to become law,” Daly says. (Last year, a long-standing proposal for a medal honoring organ donors finally became the Stephanie Tubbs-Jones Gift of Life Medal Act, after the Cleveland congresswoman died of a brain aneurysm and her family donated her organs.)
Even when you’re motivated, becoming a living donor is not as easy as it sounds—as Garet Hil discovered. Since he shares his daughter’s A blood type, he immediately agreed to give her one of his kidneys. A fit former marine without the high blood pressure that disqualifies many potential donors, he easily passed the requisite medical and psychological tests. The transplant was scheduled for May 2007.
Then, a week before surgery, a final test returned bad news. In response to a blood transfusion she’d received in the emergency room, Hil’s daughter had developed antibodies that meant she would reject his kidney. A second test confirmed the result. Worse, the three uncles who’d stepped up as substitute donors ran into the same problem. So did a “nondirected donor,” a stranger who’d agreed to give a kidney to anyone the transplant center designated. “We had five donors who failed in the course of four weeks,” Hil recalls.
Hil and his wife went on a campaign to find a new donor, calling every relative and friend they could think of. Finally, the 23-year-old son of one of Garet Hil’s brothers proved an ideal match. The transplant was done in July 2007. Two years later, both patients are doing well.
For most families, that would be the happy end of the story. But Hil wants to make sure that when his daughter’s new kidney fails in 10 or 20 years, she can get another one quickly: “When my daughter got sick and needed a transplant, I said, ‘What am I going to do so that I can help her the rest of her life?’” He is by nature a problem-solver, someone intent on developing and applying analytical tools. During his search for a kidney, he saw a lot of problems. “I learned how screwed up the system was, and I said, ‘I’m going to fix it,’” Hil recalls. “And that’s when we launched the National Kidney Registry.”
With offices in a converted colonial house on Long Island, the nonprofit registry is a modest affair—just three employees and Hil, who volunteers about 10 hours a week. Directly and indirectly (by covering the costs of computer programming and other services through Hil’s consulting company), Hil and his wife have provided most of the registry’s start-up funding, nearly $1 million. The organization’s largest outside supporter is the Aetna Foundation, which announced a $50,000 donation in March. Along with similar organizations at a few transplant centers, the registry could shorten the waiting list by significantly increasing the number of living donations.
The National Organ Transplant Act forbids offering “valuable consideration,” generally construed as cash or an equivalent quid pro quo, for an organ. But very few people are willing to give someone a kidney without getting something in return. Last year, 106 people anonymously donated kidneys to transplant centers as nondirected donors; a few more gave kidneys to people they’d met online but hadn’t previously known. But almost all living donors are helping a relative or friend. Although many people call these donations “altruistic,” they in fact offer donors a substantial benefit: saving someone they care about.
Thousands of people on the waiting list have someone who cares enough to give them a kidney but who has the wrong blood type or, like Hil, triggers antibodies in a “sensitized” kidney patient. “Imagine the frustration of watching your sister die of kidney failure, being willing and healthy enough to donate to her and give her back her life, but being denied the opportunity to do so because of some ‘antibody issue.’ Devastating,” says Dorry Segev, the director of clinical research in transplant surgery at Johns Hopkins. Until recently, the only option open to these would-be donors was to give a kidney to a transplant center’s waiting list in exchange for a deceased-donor kidney for their loved one. Since cadaver kidneys tend to go bad years before living-donor kidneys, it wasn’t an even trade. In 2008, only 99 people in the country took it.
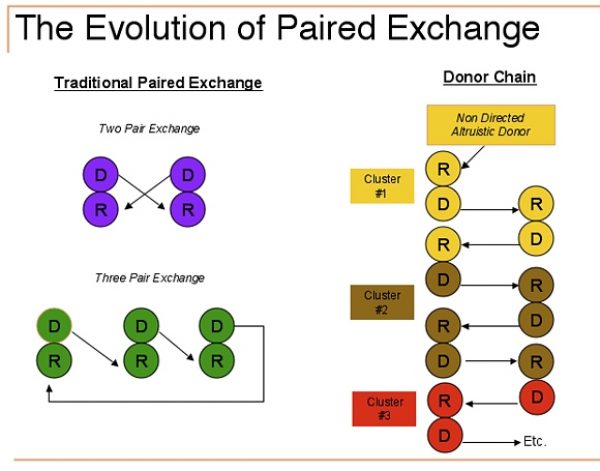
Over the past decade, however, a more promising trade has become possible. In its simplest form, known as “paired exchange,” incompatible pairs are matched. For example, a husband with type A blood wants to give a kidney to his wife, who has type B blood. Meanwhile, a mother with type B wants to donate to her son with type A. So the mother gives to the wife, and the husband gives to the son. As originally developed at Johns Hopkins, paired exchanges involved not only swaps but simultaneous surgeries, so that no one could back out. Since the first paired exchange in 2000, the number has grown from two that year to 240 in 2008 and 591 in total. (In 2007, Congress unanimously amended the law to make paired exchanges explicitly legal—but only after the bill’s original sponsor, Charlie Norwood, a Georgia congressman who’d received a lung transplant, gave the bill that all-important push. He died.)
Finding matching pairs is tricky, however, especially once you throw in the problem of sensitized recipients, who need not only the right blood type but additional antigen matches. You have to find a recipient whose incompatible donor offers what you need, and, at the same time, your donor must have exactly what that recipient needs. In his search for a kidney, Garet Hil enrolled in every existing paired-exchange program, only to discover that “my odds for getting my daughter a transplant were about 1 in 10, or 10 percent, over the next year, which was completely unacceptable.”
Bartering kidneys has the same problems as bartering anything else. What each side needs has to match perfectly. “In economics, for maybe a hundred years, people have talked about why money is important—because of the difficulties of barter. The phrase that’s come to signify that in economics is The trouble with barter is, you have to find a double coincidence of wants,” says Alvin Roth, a Harvard economist who has designed algorithms for kidney exchanges. “When you think about regular kidney exchange, what that means is, not only do we have to want your kidney; you have to want our kidney—a double coincidence of wants.” Worse, the need for simultaneous operations, requiring four operating rooms and four transplant teams, severely limits where such exchanges can be done. Paired exchange can’t significantly reduce the waiting list.
Donor chains are more promising. A donor chain starts with one of those rare (but increasingly common nondirected donors, who gives to someone who has a willing but incompatible donor. That donor then gives to someone else with an incompatible donor, who gives to a third person with an incompatible donor, and so on. In theory, a chain can go on indefinitely. The surgeries don’t have to be simultaneous, or even in the same place. In the March 12 New England Journal of Medicine, a group led by Michael A. Rees of the University of Toledo Medical Center and including Dorry Segev and Alvin Roth, reported on a chain of 10 kidney transplants involving six transplant centers in five states. If a donor drops out, whether for personal or medical reasons, the chain simply ends. The waiting recipient is disappointed, but still has an incompatible donor. They can join a new chain.
The bigger the pool of potential donors and recipients, the better the matches can be, a particularly important consideration for sensitized patients. Few kidney patients have as big a family network as Garet Hil’s daughter. Someone with diabetes, which runs in families, or polycystic kidney disease, a relatively common genetic disorder, may have only one healthy potential donor. So the National Kidney Registry aims to build as large a pool as possible, and has already signed up 28 transplant centers, including 11 of the 20 largest. The centers enter information about patients and their willing but incompatible donors into the registry’s database, making those pairs eligible for weekly “match runs” to find optimal chains.
The registry also operates as a clearinghouse for prospective nondirected donors. They first complete an online form, which screens out people with obvious disqualifying medical conditions, and get a health certificate from their doctor. Registry counselors then do phone interviews to eliminate cranks and those seeking illegal payments. Prospects who make it past the initial screening get a swab kit, originally developed for the national bone-marrow registry, so they can test their blood type and three important antigens. These steps reduce the burden on busy transplant centers, who can find dealing with prospective nondirected donors a distracting time sink.
The registry has facilitated 44 transplants since its first, on Valentine’s Day 2008, including 23 in the first six months of 2009, with 42 more expected this year. More than 1,200 people have completed the online form. While most back out or are disqualified for medical reasons, notably high blood pressure or obesity, the registry so far has attracted plenty of the nondirected donors. Forty applicants have passed the initial screening and completed the swab test, and 20 have gone through full workups. Sixteen of those have already completed registry-facilitated transplants. “There are apparently a lot of people in the United States willing to donate their kidney to a stranger,” says Hil.
A chain makes that gift even more appealing, since the nondirected donor helps not just one person but a whole series of patients. “It allows the generosity of nondirected donors to be multiplied over and over again. They become like a spark for a fire,” says Gabriel Danovitch, the medical director of the kidney-and-pancreas transplant program at UCLA, one of the National Kidney Registry’s affiliate centers. Danovitch, who admits he originally wasn’t quite sure what to make of this entrepreneurial outsider, now says he has “great respect” for Hil, adding that UCLA has “had a very, very good experience” with the registry.
Donor chains represent a cultural shift in the world of transplants, away from rationing cadaver organs and toward searching for living donors, away from using whatever living donor is available and toward finding the best possible match. They also mean embracing a relatively new idea: strangers giving kidneys to strangers. Above all, chains represent a much-needed sense of urgency, a growing conviction that rewarding patients for stoically waiting their turn as their health deteriorates is unjustified and unnecessary.
But at transplant centers, that urgency is still mostly theoretical. Despite waiting lists numbering in the thousands, the 28 centers enrolled in the National Kidney Registry have listed a mere 152 incompatible pairs—so few that the registry actually has extra type A donors with no one to take their kidneys. “We’ve got donors right now waiting for recipients who don’t know that we’re out there. We could get these people transplanted immediately, and they don’t know that we exist,” says Hil. “Either the transplant centers haven’t told them, or the transplant centers don’t know” the registry has donors waiting. “It’s mind-boggling.”
To make chains more than a clever concept, transplant centers need to start routinely recording information on willing but incompatible donors and entering it in databases for matching. “Almost every potential donor could be a donor if our current knowledge was maximized,” says UCLA’s Danovitch. But once potential donors are deemed incompatible, most of them simply get lost. “We’re nowhere near maximizing at the moment,” he says. “We’re just dipping our toes in the water, essentially, compared to what could be done.”
Danovitch is surely correct that transplant centers could move many more patients off the waiting list if they put more patients and potential donors into a central registry and took full advantage of chains. But all of this mathematical ingenuity and institutional transformation can only go so far. Eventually the need for that “double coincidence of wants” limits even the most sophisticated barter chains. The most wildly optimistic estimates suggest that perhaps 15,000 patients on the waiting list have willing but incompatible donors. That leaves another 65,000 who have nothing to swap. Donor chains discriminate against people with small families, bad genetics, or sick friends.
“My sister offered, but she’s diabetic. My wife offered, but she’s diabetic,” Henry David, the L.A. business owner, said in February. “My older son was born with hydronephrosis, which is a kinked ureter,” so his kidney is only partially functioning. “I’ve got another son, but with the crappy genetics, I haven’t asked him, because I figure he’s going to have trouble down the road.” For patients like David, donor chains provide only indirect help, by taking luckier people off the waiting list.
Because they deal in barter, donor chains don’t require any new laws. They aren’t especially controversial, just logistically tricky. People like Danovitch, who vehemently opposes financial incentives for donors, and people like Arthur Matas, who strongly supports such compensation, can all agree that swapping kidneys is a good thing. “Every one of these things that takes one person off dialysis and gives them a good functioning kidney is worth fighting for,” says Matas. But if the goal is to end the waiting list, chains are a compromise that falls far short.
“This paired exchange thing—can it make the list go to zero? I don’t think so,” admits Hil. But, as much as he wants to help kidney patients in general, his primary goals are personal. “My daughter needs another kidney in 20 years, and I know that she has many donors,” and thus plenty to barter with. “I can’t solve the whole problem, but if I solve half of the problem, it’s the half that’s really relevant” to helping her.
The obvious solution to the problem of barter is, of course, money. Altruistic blood donors often receive freebies like movie tickets or paid vacation hours that would be illegal for kidney donors. Plasma and sperm donors routinely receive cash, as do egg donors and surrogate mothers, who get tens of thousands of dollars.. If transplant centers could pay $25,000 or $50,000 to each living kidney donor, many more people would line up to contribute.
Such payments could even save taxpayers billions of dollars. Long-term dialysis is a federal entitlement. Under a special law, Medicare covers everyone, regardless of age, who has made minimal Social Security tax payments—about 319,000 of the country’s 400,000 dialysis patients. Compared with dialysis payments, every transplant from a living, unrelated donor saves an expected present value of almost $100,000 in medical costs, according to a 2003 American Journal of Transplantation article by Matas and Mark Schnitzler, an economist then at Washington University in St. Louis and now at the Saint Louis University Center for Outcomes Research.
Eliminating the waiting list would thus save taxpayers $8 billion, or $4 billion if each living donor received a lump-sum payment of $50,000.
That purely financial estimate ignores the enormous benefits for the patients’ quality of life, of course. It also excludes the economic gains from returning to productive work—only about 10 percent of dialysis patients are employed even part-time—and the fiscal effects of paying taxes rather than receiving disability payments.
Registries and chains provide a model for how an above-board market in kidneys might develop, protecting the interests of both donors and recipients. Just as the National Kidney Registry initially screens nondirected altruistic donors, a central organization could do the same for prospective kidney vendors. Those who qualified would be referred to local transplant centers for full medical and psychological testing, after which they could be matched with the recipients—and possibly chains—for whom they were best suited. Unlike volunteers, vendors would not get to choose their recipients, giving everyone in need of a kidney a fair shot. Payment would come not from individual recipients but, as for the rest of the transplant process, through normal insurance (including Medicare) at standard rates.
Such proposals, of course, attract vehement opposition from people who fear that financial incentives would squeeze out unpaid donors, entice the poor into bad medical choices, or “cheapen the gift.” Some volunteers would undoubtedly drop out, relieved to let someone else provide their loved one’s new kidney. But real incentives, rather than token rewards, would produce a net increase in the number of transplants. Giving a kidney to a relative or friend could still speed up the process, providing an incentive to do so but relieving such donors of any sense of emotional blackmail.
A well-designed system could address the concerns about donor welfare by including educational programs, waiting periods, and follow-up care for donors, and possibly by allocating the payments over time rather than offering immediate cash. As for “cheapening” donation, Matas notes the importance of attitude. “We need to create a culture of dignity. There are many people who want to do this, and the incentive would push them over the edge,” he says. “The message should be, ‘We can compensate you but never repay you.’”
Outlawing payments to donors is ostensibly a way to keep the system fair, giving rich and poor an equally lousy chance of getting a kidney. But wealthier people can already more easily register at distant centers with short lists. They’re also more likely to have friends and relatives who can afford the nonmedical expenses that living donation often entails, including time off from work, child care, hotel rooms, or cross-country travel. (It is legal for recipients or third parties to pay such expenses, but, unlike medical costs, they are not covered by insurance.)
Patients with enough money and the right networks have yet another option. They can go abroad, to countries where the authorities sanction or ignore payments to living donors. That’s how Henry David got his new kidney.
A cousin in Canada referred him to a close friend who’d received a transplant overseas two years ago, with excellent surgical care and good results. David contacted the surgeon, sent his medical records, and after a few delays flew to Israel for the final workup and then to a country he doesn’t want identified for the transplant. He saw the donor, a 31-year-old man, who stayed with two other donor friends in an adjacent hospital room, but did not talk to him. (Neither spoke the other’s language.) David paid $120,000 out of pocket for the full procedure. He believes $30,000 went to the donor. Because of the shadowy, international nature of the operation, however, he cannot be sure.
Such “transplant tourism” is growing. Many of the transplants are not as medically sound as David’s, and the care for living donors, even when adequate, rarely meets U.S. standards. Laparoscopic surgery is a First World luxury, as are desk jobs to which donors can safely return soon after surgery. With few protections beyond the surgeon’s need to maintain a good reputation among potential donors, kidney vendors may not receive the full payments they’re promised. In China (which is not where David went), organs may come not only from paid living vendors but also from executed prisoners. Transplant tourism is, in short, an ethical morass.
It is also a completely predictable byproduct of the current system, willed into being by policy makers who ignore the plight of kidney patients and by doctors who see above-board payments—and the protections of contract and malpractice law that would go with them—as pollution. Living donation is a low-risk procedure for the donor that offers life-changing rewards for the recipient. Yet the donor is the only person involved in the process who receives no compensation. “There’s no reason that someone who does this should not get something substantial that will make a difference in their lives,” says David. To people who like to celebrate living donors as heroes, payment seems terribly crass. But the vicarious thrill of someone else’s altruism comes at a terrible cost.